Connect With Us
Blog
Blog
How Do Walking and Running Shoes Differ?

Running and walking shoes may appear similar, but they are designed with distinct features to support different types of movement. Running shoes typically offer more cushioning to absorb the higher impact forces generated with each stride. They often have a higher heel height and a noticeable heel flare to provide stability during forward motion and shock absorption during heel strike. Walking shoes have less cushioning and a lower heel profile, as walking produces less impact. They also offer more flexibility through the forefoot to support the natural rolling motion of the foot. Using the correct shoe for each activity helps reduce the risk of discomfort and injury. If you have developed foot pain from wearing the wrong shoes for walking or running, it is suggested that you contact a podiatrist who can treat various foot conditions.
Finding a properly-fitting shoe is important in reducing injuries and preventing foot problems. For more information about treatment, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
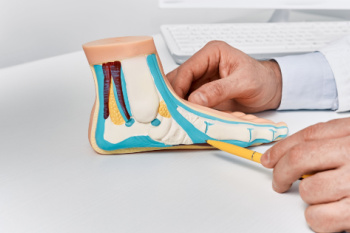
Proper Shoe Fitting
A common concern when it comes to foot health, having properly fitted shoes can help prevent injuries to the foot. Out feet affect our posture and gait, which in turn affects the biomechanics and overall bodily structure. With 33 joints, 26 bones, and over 100 ligaments, the potential for serious injury is much greater than one realizes. Although the feet cease growth in adulthood, they still change shape as they mature. Here are some factors to consider when it comes to investing in proper fitting shoes:
- Be sure the shoes fit correctly right away
- Ensure the ball of your foot fits comfortably in the widest portion of the shoes
- Even though they may look fashionable, improper fitting shoes can either create adverse conditions or exacerbate existing ones you may already have
- Walk along a carpeted surface to ensure the shoes comfortably fit during normal activity
Keeping in mind how shoes fit the biomechanics of your body, properly-fitting shoes are vitally important. Fortunately, it is not difficult to acquire footwear that fits correctly. Be sure to wear shoes that support the overall structure of your body. Do your feet a favor and invest in several pairs of well-fitted shoes today.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
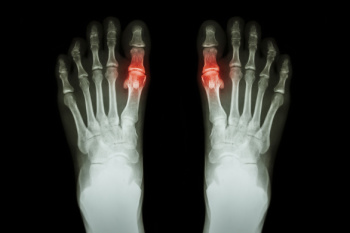
Types of Toe Fractures

Toe fractures usually result from direct trauma, such as stubbing the toe or dropping something on the foot. The most frequently affected areas are the lesser toes, especially the part of the toe closest to the rest of the foot. Types of toe fractures include simple fractures, where the bone remains intact under the skin, and compound fractures, where the bone breaks through the skin and may lead to infection. Avulsion fractures occur when a tendon or ligament pulls a piece of bone away, while comminuted fractures involve the bone shattering into multiple fragments. Intra-articular fractures extend into the joint and may affect long-term toe mobility, and dislocation fractures combine a bone break with joint misalignment. A podiatrist can assess the injury using imaging such as X-rays to determine the type of fracture and the degree of bone displacement. Treatment may involve immobilization with a cast or walking boot, or in more severe cases, surgery to realign and secure the bones. If you have broken or severely bruised your toe, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Enhancing Functional Fitness with Foot Exercises

Foot exercises play a vital role in maintaining strength, flexibility, and stability for everyday movement. Strong and flexible feet improve balance, posture, and overall mobility. The alphabet exercise, where the foot traces letters in the air, helps with ankle flexibility and coordination. Towel scrunches strengthen the arch and toes by gripping a towel with the toes. Toe pointing enhances foot control and muscle engagement, while toe stretching relieves tension and promotes flexibility. These exercises support functional fitness by preventing injuries, improving endurance, and enhancing performance in daily activities. Regular foot strengthening and stretching help maintain proper alignment and reduce strain on other joints. If you have foot pain, it is suggested that you visit a podiatrist who can treat various foot conditions, and guide you on appropriate foot exercises for overall health.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Painful Gout Attacks at Night
Gout attacks at night can be particularly debilitating, causing severe pain, swelling, and redness in the feet that can interfere with sleep. This form of arthritis is caused by a buildup of uric acid in the joints, often targeting the big toe, which is more susceptible to stress and cooler temperatures. Factors such as dehydration, lower body temperature, and reduced cortisol levels during sleep, can trigger these nighttime flare-ups. The pain from a gout attack can be so intense that finding relief becomes a challenge without professional help. A podiatrist can evaluate your symptoms, confirm the diagnosis, and provide treatment to help prevent future flare-ups. Recommendations may include lifestyle adjustments like dietary changes, weight management, and anti-inflammatory treatments to ease pain and swelling. Effectively managing gout not only helps protect your feet and joints but also promotes better sleep. If you are struggling with painful gout attacks at night, it is suggested that you schedule an appointment with a podiatrist.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Warts Can Be Treated!
Understanding Sever’s Disease
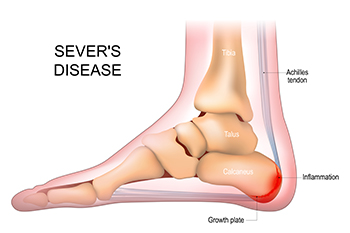
Sever’s disease is a common cause of heel pain in growing children, particularly those who are active in sports. It occurs when the growth plate in the heel becomes inflamed due to repetitive stress and tension from the Achilles tendon. This condition is most common during periods of rapid growth, when bones lengthen faster than muscles and tendons can adapt. Causes include excessive running, jumping, and footwear that lacks adequate support. Symptoms include pain and tenderness at the back of the heel, swelling, and difficulty walking or participating in physical activities. The discomfort may worsen with activity and improve with rest. If your active child has heel pain, it is suggested that you consult a podiatrist who can accurately diagnose and manage Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Concerns and Conditions Affecting Children’s Feet

Children’s foot health is essential for their overall growth and development. Common conditions that may affect their feet include bowed legs, flat feet, in-toeing, out-toeing, and curly toes. Bowed legs are often seen in toddlers and usually resolve as they grow. Flat feet, where the arch does not develop properly, may cause discomfort or pain but often improve with age. In-toeing and out-toeing, where the feet turn inward or outward while walking, can be normal in young children but may need attention if they persist. Additionally, curly toes, where one or more toes bend toward others, can cause irritation or difficulty finding comfortable shoes. If your child has any kind of foot condition, it is suggested that you consult a podiatrist who can offer appropriate treatment solutions.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Changes During Pregnancy

Pregnancy brings significant changes to the body, including the feet. Increased foot size is common due to hormonal changes that relax ligaments, causing the arches to flatten and the feet to lengthen. Many women experience heel pain and plantar fasciitis as extra weight places stress on the foot’s supportive structures. Swollen feet result from fluid retention and reduced circulation, leading to discomfort and tightness in shoes. Balance issues may arise as the center of gravity shifts, making walking more challenging. Additionally, flat feet can develop as the arches lose support, leading to fatigue and strain. Wearing supportive footwear, staying hydrated, and elevating the feet can help alleviate discomfort. If you are experiencing foot pain during your pregnancy, it is suggested that you consult a podiatrist who can determine what the cause is, and offer effective relief tips.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Role of Dermatophytes in Athlete’s Foot

Athlete's foot is a skin infection caused by dermatophytes, a type of mould-like fungus. These tiny organisms thrive in warm, damp environments, such as locker rooms, public showers, and sweaty athletic shoes. When feet remain moist for long periods, dermatophytes can easily invade the skin, leading to irritation, itching, and redness between the toes and the soles. The fungus may spread rapidly if not properly treated, resulting in discomfort and persistent infections. Maintaining dry feet, wearing breathable footwear, and practicing good hygiene can help prevent this condition. Early signs include mild scaling and burning sensations. Recognizing the symptoms and acting quickly can reduce the risk of further complications. If discomfort continues or the infection worsens, it is suggested that you see a podiatrist for proper diagnosis and appropriate treatment.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why Ankles Hurt from Running and How to Prevent It

Ankle pain from running is often caused by overuse, wearing improper footwear, weak stabilizing muscles, or biomechanical issues. The repetitive impact of running places stress on the ankle joints, tendons, and ligaments, leading to inflammation or strain. Uneven surfaces and improper running form can also contribute to discomfort. Wearing supportive shoes with proper cushioning and ensuring a good fit can reduce stress on the ankles. Strengthening exercises for the lower leg and foot muscles help improve stability and reduce the risk of an ankle injury. Stretching before and after a run promotes flexibility and prevents stiffness. Gradually increasing intensity rather than making sudden changes in distance or speed allows the body to adapt. Rest can alleviate minor soreness, while persistent pain may require medical attention. If you have endured an ankle injury from running, it is suggested that you consult a podiatrist who can offer effective treatment and running injury prevention solutions.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
More...
Do You Suffer From Painful Feet?
What Is a Disappearing Nail Bed?

A disappearing nail bed, or DNB, is a rare condition where the nail plate begins to shrink or detach from the nail bed, often leading to nail loss or deformation. DNB can be caused by trauma, fungal infections, poor circulation, or certain skin conditions like psoriasis. It is more common in people with underlying health issues, such as diabetes or autoimmune disorders. The symptoms of DNB include pain or discomfort surrounding he nail, thinning or ridged nails, and a visible gap between the nail and nail bed. The area may look discolored or flaky, and in severe cases, the nail may fall off completely. Treatment for DNB focuses on addressing the underlying cause. A podiatrist may recommend topical treatments, proper nail care, or antibiotics if an infection is present. If the condition is caused by trauma or circulation issues, they may discuss ways to promote healing and prevent further nail loss. If you are experiencing changes in your nails, it is suggested that you schedule an appointment with a podiatrist to get an accurate diagnosis and effective treatment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Facts About Heel Spurs

A heel spur is a bony growth that develops on the underside of the heel bone, typically caused by repetitive stress or pressure. This condition is often associated with plantar fasciitis, where inflammation occurs in the thick band of tissue connecting the heel to the toes. Heel spurs are usually the result of constant stress on the feet, which can occur from activities such as running, walking, or standing for long periods. The most common symptoms of heel spurs include sharp pain at the heel, especially in the morning or after periods of rest. Swelling and tenderness may also accompany the condition. Over time, the pain may subside but can reoccur during physical activities. Treatment options include rest, stretches, and in some cases, orthotics or surgery if conservative measures do not provide relief. If you have heel pain, it is suggested that you consult a podiatrist who can do an examination and provide an accurate diagnosis and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the latest in diagnostic and treatment technology to meet your needs.
Facts About Flat Feet
Flat feet, or pes planus, occur when the arches of the feet are absent, causing the entire sole to make contact with the ground. This condition is common among infants and toddlers, but typically resolves as the tendons and ligaments strengthen during early childhood. For some people, flat feet persist into adulthood or develop later due to injuries, aging, or conditions such as posterior tibial tendon dysfunction. Symptoms can range from no discomfort to pain in the feet, ankles, or lower legs, especially after prolonged standing or physical activity. Tight Achilles tendons and damage to the tendons that support the arch can contribute to flat feet, making walking and running uncomfortable. In cases where flat feet lead to significant pain or mobility issues, a podiatrist can use imaging tests and physical assessments to assess the severity. Treatment may include custom orthotics, shoe modifications, or in severe cases, surgery to repair or support the foot’s structure. If you have foot problems related to flat feet, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019