Connect With Us
Blog

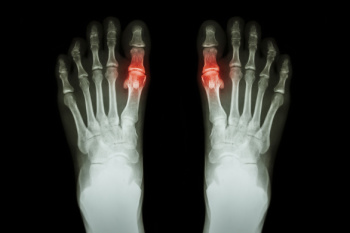
Toe fractures usually result from direct trauma, such as stubbing the toe or dropping something on the foot. The most frequently affected areas are the lesser toes, especially the part of the toe closest to the rest of the foot. Types of toe fractures include simple fractures, where the bone remains intact under the skin, and compound fractures, where the bone breaks through the skin and may lead to infection. Avulsion fractures occur when a tendon or ligament pulls a piece of bone away, while comminuted fractures involve the bone shattering into multiple fragments. Intra-articular fractures extend into the joint and may affect long-term toe mobility, and dislocation fractures combine a bone break with joint misalignment. A podiatrist can assess the injury using imaging such as X-rays to determine the type of fracture and the degree of bone displacement. Treatment may involve immobilization with a cast or walking boot, or in more severe cases, surgery to realign and secure the bones. If you have broken or severely bruised your toe, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Foot exercises play a vital role in maintaining strength, flexibility, and stability for everyday movement. Strong and flexible feet improve balance, posture, and overall mobility. The alphabet exercise, where the foot traces letters in the air, helps with ankle flexibility and coordination. Towel scrunches strengthen the arch and toes by gripping a towel with the toes. Toe pointing enhances foot control and muscle engagement, while toe stretching relieves tension and promotes flexibility. These exercises support functional fitness by preventing injuries, improving endurance, and enhancing performance in daily activities. Regular foot strengthening and stretching help maintain proper alignment and reduce strain on other joints. If you have foot pain, it is suggested that you visit a podiatrist who can treat various foot conditions, and guide you on appropriate foot exercises for overall health.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Gout attacks at night can be particularly debilitating, causing severe pain, swelling, and redness in the feet that can interfere with sleep. This form of arthritis is caused by a buildup of uric acid in the joints, often targeting the big toe, which is more susceptible to stress and cooler temperatures. Factors such as dehydration, lower body temperature, and reduced cortisol levels during sleep, can trigger these nighttime flare-ups. The pain from a gout attack can be so intense that finding relief becomes a challenge without professional help. A podiatrist can evaluate your symptoms, confirm the diagnosis, and provide treatment to help prevent future flare-ups. Recommendations may include lifestyle adjustments like dietary changes, weight management, and anti-inflammatory treatments to ease pain and swelling. Effectively managing gout not only helps protect your feet and joints but also promotes better sleep. If you are struggling with painful gout attacks at night, it is suggested that you schedule an appointment with a podiatrist.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019