Connect With Us
Blog
Blog
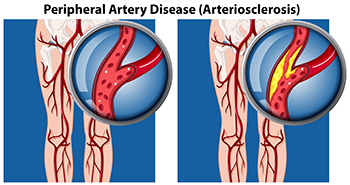
Peripheral Artery Disease Explained
Peripheral artery disease (PAD) is a medical condition that can cause poor circulation in the lower limbs. This occurs due to a buildup of fatty plaques in the arteries that supply the lower limbs. The plaque causes arteries to narrow and harden, making it more difficult for blood to travel through them and bring oxygen and nutrients to the feet and ankles. In its early stages, PAD may be asymptomatic. As it progresses, symptoms can include foot and leg cramps, numbness, weakness, coldness, skin discoloration, hair loss, and slow-healing sores and wounds on the lower limbs. Your podiatrist can screen you for PAD through a variety of simple, noninvasive tests. If you suspect that you may have PAD, or if you are an older adult or have a family history of vascular disease, it is suggested that you visit a podiatrist for a PAD screening.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Is the Tarsal Tunnel and Why Is It Causing Me Pain?
The tarsal tunnel is a narrow passageway on the inside of the ankle that is made of a thick band of fibrous tissue (flexor retinaculum) and ankle bones. Veins, arteries, muscles, tendons, and the tibial nerve pass through the tarsal tunnel. Certain conditions such as a ganglion cyst, nerve sheath tumors, fibrosis, and even injuries can tighten the already-narrow space within the tunnel and compress the tibial nerve. This can cause burning pain or tingling (paresthesias) along the tibial nerve, the inside of the ankle, or bottom (plantar) part of the foot. If you are experiencing this type of discomfort, contact a podiatrist. They will perform a physical examination and may suggest that an MRI be performed to visualize lesions that may be present within the tunnel. Both conservative and surgical treatments will be considered depending on the cause and severity of the condition and will focus on reducing pressure on the nerve and relieving pain.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain Can Be Treated!
Why You Should Never Ignore Any Fracture in Your Toe
Fractures in the toes and metatarsals (long bones in the midfoot that connect to the toe bones) can be quite painful and should not be taken lightly. Breaks can either be traumatic (acute) that occur instantly due to an injury, or can be stress fractures which develop over time. Traumatic fractures can cause a bone to become misaligned in certain cases. You may hear a snap at the moment of impact and you may even notice that the toe is crooked or misshapen in some way. Pain may be felt at the site of the injury, and bruising and swelling may occur the following day. With a stress fracture, any pain felt while using the affected foot may subside when you rest, and although you may notice swelling there should be no apparent bruising. It is important to see a podiatrist for any broken bone in your toe or metatarsal, even if you have been treated initially at an emergency room. Proper treatment and rehabilitation will help avoid future complications like an improperly healed bone, mobility issues, difficulty wearing shoes, deformities, chronic pain, or arthritis in the joint.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Keeping Your Heels Soft to Prevent Them From Cracking
When you apply weight to your foot, the skin on your heels expands. If this skin is dry and lacking elasticity, cracks in the skin may eventually form. Dry, cold weather, obesity, open-back shoes, standing on hard floors for an extended period of time, and conditions that cause dry skin can all contribute to heels becoming stiff and cracked. To avoid getting cracked heels, keep them moisturized. The best way to seal in moisture is to apply ointment or cream—containing hyaluronic or lactic acid, mineral oil, lanolin or petrolatum—right after a shower or bath. If your heels are already thickened and cracked, you can try to thin them down by gently rubbing them with a pumice stone or applying a keratolytic agent, unless you have diabetes, nerve damage, or poor circulation. If cracked heels are allowed to deepen, they may become painful and bleed, and possibly even become infected. If your cracked heels have progressed to this point, or you need help getting them smooth and supple again, make an appointment with your local podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
When Your Ankle Twists Too Far
If you’ve ever stepped off a curb or jumped and landed awkwardly, you may have felt your ankle twist. Sometimes, an ankle can twist so much that the ligaments that support the ankle become overstretched or torn. When this happens, it is known as an ankle sprain. Ankle sprains range in severity, but symptoms usually include ankle pain, tenderness, swelling, and bruising. The more damaged the ligaments, the worse the symptoms. In more severe sprains, it may be difficult or impossible to walk due to ankle pain and instability. The ankle may also have a restricted range of motion. If you suspect that you have sprained your ankle, it is suggested that you seek the care of a podiatrist as soon as possible.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts Can Be Treated!
An Athlete’s Foot Overview
Athlete’s foot or Tinea Pedis, is a fungal infection that can produce a red, itchy, stinging, flaky rash on the uppermost layer of skin between the toes and on top of the foot. The microorganism responsible for Athlete’s foot is called Trichophyton, which loves moist, warm environments. Athlete’s foot can spread through skin-to-skin contact at the site where the fungus lives. It can also spread indirectly, through contact with a contaminated area or object such as shoes, towels, socks and more. Untreated Athlete’s foot may spread the infection from toe to toe, or even to the hands in rare cases. If you believe you have Athlete’s foot call a podiatrist as soon as possible to determine what treatment option is best for you.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Abnormal Gaits
An abnormal gait is a dysfunctional walking pattern. It typically occurs due to biomechanical problems win the feet and ankles. In a normal gait, the feet both spend roughly an equal amount of time in contact with the ground. Many patients complain of a painful (antalgic) gait. This type of gait is usually due to a foot or ankle injury. The patient avoids bearing weight on the injured foot, resulting in an altered gait with shorter strides and an inequality in the amount of time each foot spends in contact with the ground (with the injured foot on the ground less). A high steppage gait is a walking pattern characterized by bending the knee more than is normal while walking. Patients do this to compensate for weak anterior compartment muscles, which can cause their foot to drop or slap onto the ground. If you have an abnormal gait, it is strongly suggested that you see a podiatrist for diagnosis and treatment.
If you have any concerns about your feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Stretches for the Sole
 The plantar fascia is a ligament that runs along the bottom of each foot, connecting the heel bone to the toes. When this ligament is injured or inflamed, the result is usually heel and arch pain. One way to prevent or relieve tension and pain in the heel, arch, and sole of the foot is by stretching. To stretch the plantar fascia and relieve tightness under the foot, you can do a foot pull. Sit with one leg crossed over the other, then grab all of your toes and pull them as a unit back towards your shin, until you feel a pull in the bottom of your foot. Hold for 10 seconds and repeat 10 times. To massage the plantar fascia, roll a tennis ball forward and back with the bottom of your foot for 5-10 minutes a day. To learn more about plantar fascia stretches, please consult with a podiatrist.
The plantar fascia is a ligament that runs along the bottom of each foot, connecting the heel bone to the toes. When this ligament is injured or inflamed, the result is usually heel and arch pain. One way to prevent or relieve tension and pain in the heel, arch, and sole of the foot is by stretching. To stretch the plantar fascia and relieve tightness under the foot, you can do a foot pull. Sit with one leg crossed over the other, then grab all of your toes and pull them as a unit back towards your shin, until you feel a pull in the bottom of your foot. Hold for 10 seconds and repeat 10 times. To massage the plantar fascia, roll a tennis ball forward and back with the bottom of your foot for 5-10 minutes a day. To learn more about plantar fascia stretches, please consult with a podiatrist.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Being the backbone of the body, the feet carry your entire weight and can easily become overexerted, causing cramps and pain. As with any body part, stretching your feet can serve many benefits. From increasing flexibility to even providing some pain relief, be sure to give your feet a stretch from time to time. This is especially important for athletes or anyone performing aerobic exercises, but anyone experiencing foot pain or is on their feet constantly should also engage in this practice.
Great ways to stretch your feet:
- Crossing one leg over the others and carefully pull your toes back. Do 10-20 repetitions and repeat the process for each foot
- Face a wall with your arms out and hands flat against the wall. Step back with one foot and keep it flat on the floor while moving the other leg forward. Lean towards the wall until you feel a stretch. Hold for 30 seconds and perform 10 repetitions for each foot
- Be sure not to overextend or push your limbs too hard or you could risk pulling or straining your muscle
Individuals who tend to their feet by regular stretching every day should be able to minimize foot pain and prevent new problems from arising.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
More...
Making Sense of Pinky Toe Pain
Discovering the cause of pinky toe pain can be challenging. Its strategic placement on the outside of the foot helps the pinky toe work in tandem with the heel and big toe to balance the body during movement. However, this very location and its petite size make the pinky toe more susceptible to injury. For instance, stubbing, or dropping something heavy on it can cause one or more of its three bones to break. Stress, or hairline, fractures may also occur from repeated motions and activities such as running and jumping. One of its bones may separate from the others, causing dislocation (complete separation), or subluxation (partial separation). If ligaments become damaged, this can result in a sprain. Other conditions that may cause pinky toe pain include tailor’s bunions (a bunionette that forms on the outside of the pinky toe), or deformities such as hammer toe, claw toe, or overlapping pinky toe. Any chronic pain, swelling, or malformation in your pinky toe should be diagnosed by a podiatrist, followed by an appropriate course of treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Causes Cracked Heels?
 When the skin on the heel dries out and loses its strength and elasticity, the heel becomes hard, dry, and flaky. This leads to splitting, or fissuring and cracking, of skin around the heel which is more commonly known as cracked heels. While cracked heels usually form because of dry skin, wearing open-backed shoes, gaining weight, and increased friction from the back of the shoes can all lead to cracked heels forming as well. Common methods for managing cracked heels include moisturizing the heels twice per day, soaking the feet in warm water, and using a pumice stone on the affected area. However, excessively dry skin can indicate other problems such as neuropathy or diabetes. Patients who continually struggle with cracked heels should consult with a podiatrist to find the source of their issue.
When the skin on the heel dries out and loses its strength and elasticity, the heel becomes hard, dry, and flaky. This leads to splitting, or fissuring and cracking, of skin around the heel which is more commonly known as cracked heels. While cracked heels usually form because of dry skin, wearing open-backed shoes, gaining weight, and increased friction from the back of the shoes can all lead to cracked heels forming as well. Common methods for managing cracked heels include moisturizing the heels twice per day, soaking the feet in warm water, and using a pumice stone on the affected area. However, excessively dry skin can indicate other problems such as neuropathy or diabetes. Patients who continually struggle with cracked heels should consult with a podiatrist to find the source of their issue.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
PAD Symptoms and Risk Factors
Peripheral artery disease (PAD) is a condition characterized by poor circulation in the lower limbs. It occurs when the arteries that transport blood in the lower limbs become narrow and hardened due to a buildup of plaque. In its earlier stages, PAD is often asymptomatic. As it progresses, symptoms can begin to appear and may include leg cramping, numbness, weakness, coldness, discoloration, hair loss, changes in the texture and color of toenails, and the formation of poorly healing wounds on the feet and ankles. Since symptoms might not arise until the disease has progressed significantly, screening for PAD is very important. People who are at risk for PAD, such as adults over the age of 50, those who live a sedentary lifestyle, and those who have a history of diabetes, high blood pressure, high cholesterol, or cardiovascular problems, should speak with a podiatrist about getting tested for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Do You Suffer From Painful Feet?
Blog Archives
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019