Connect With Us
Blog
Items filtered by date: June 2021
Children Limping May Indicate Sever’s Disease
 Active children may be more likely to experience heel pain. This pain can be indicative of a condition known as Sever’s disease, and can target children and young adolescents. This uncomfortable ailment affects the growth plate in the heel and can occur as a result of extensive pressure exerted on the area where the Achilles tendon meets the heel. Parents may notice their child may begin to limp, in addition to experiencing a decrease in flexibility if their child is afflicted with Sever’s disease. Prompt treatment generally begins with stopping the activity that caused this condition, and it is beneficial to rest the affected foot. Some children find it may help to perform specific stretches that target the Achilles tendon and calf. If you notice your child has symptoms of Sever’s disease, it is strongly suggested that you schedule a consultation with a podiatrist as quickly as possible who can determine what the most effective treatment is.
Active children may be more likely to experience heel pain. This pain can be indicative of a condition known as Sever’s disease, and can target children and young adolescents. This uncomfortable ailment affects the growth plate in the heel and can occur as a result of extensive pressure exerted on the area where the Achilles tendon meets the heel. Parents may notice their child may begin to limp, in addition to experiencing a decrease in flexibility if their child is afflicted with Sever’s disease. Prompt treatment generally begins with stopping the activity that caused this condition, and it is beneficial to rest the affected foot. Some children find it may help to perform specific stretches that target the Achilles tendon and calf. If you notice your child has symptoms of Sever’s disease, it is strongly suggested that you schedule a consultation with a podiatrist as quickly as possible who can determine what the most effective treatment is.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
What Can Cause Burning Pain in the Ball of Your Foot?
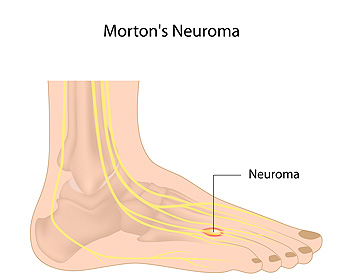
Morton’s neuroma is often caused by high heels or tight shoes which can pinch toes together, causing nerves to become compressed or aggravated and thickened in response to the irritation. Aside from improper footwear, other factors—such as having flat feet, bunions, hammertoes, high arches, or participating in certain sports activities—may also put pressure on the nerves between the toes and contribute to the development of Morton’s neuroma. This condition most typically occurs between the third and fourth toes, but may also develop between the second and third toes. Symptoms of Morton’s neuroma may include a feeling of having a marble or pebble in your shoe, a burning sensation in the ball of your foot, numb toes, pain radiating from your toes, or trouble walking. Sometimes people with Morton’s neuroma have no symptoms at all. If you suspect you may have Morton’s neuroma, seek the care of a podiatrist for an examination, diagnosis and treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Common Bunion Treatments and What They Do
 Bunions are bony bumps that form on the sides of the big toes, at the base of the big toe joint. They are a common deformity that can push the big toe towards the other toes and make wearing shoes uncomfortable. While bunions can be surgically corrected, your doctor will usually suggest non-surgical treatments first. These treatments won’t cure the bunion, but they will relieve symptoms and can stop the bunion from getting worse. Wearing shoes with low heels and a wide toe box is helpful for relieving pressure on the bunion and makes walking more comfortable. Wearing orthotic inserts in your shoes can help support the foot and improve its alignment. Wearing a toe splint at night immobilizes the toe and holds it in a straighter position. Putting an ice pack on the bunion can help reduce swelling and pain. If you have bunions, please see a podiatrist to learn about more treatment options and find the right ones for you.
Bunions are bony bumps that form on the sides of the big toes, at the base of the big toe joint. They are a common deformity that can push the big toe towards the other toes and make wearing shoes uncomfortable. While bunions can be surgically corrected, your doctor will usually suggest non-surgical treatments first. These treatments won’t cure the bunion, but they will relieve symptoms and can stop the bunion from getting worse. Wearing shoes with low heels and a wide toe box is helpful for relieving pressure on the bunion and makes walking more comfortable. Wearing orthotic inserts in your shoes can help support the foot and improve its alignment. Wearing a toe splint at night immobilizes the toe and holds it in a straighter position. Putting an ice pack on the bunion can help reduce swelling and pain. If you have bunions, please see a podiatrist to learn about more treatment options and find the right ones for you.
If you are suffering from bunions, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
What Are the Symptoms of Tarsal Tunnel Syndrome?
 Tarsal tunnel syndrome may not be a commonly known ailment, but have you heard of carpal tunnel syndrome? Carpal tunnel affects the hands while tarsal tunnel syndrome occurs in the feet and can cause pain and discomfort. Research has indicated that people who have arthritis may be prone to developing this condition, in addition to frequently enduring high-stress activities. Some of the symptoms that are associated with this ailment often include tired feet and ankles, and the overall foot may be numb or have tingling sensations. Some patients have pain in the Achilles tendon area, and the ankles may appear swollen. There are several symptoms that can be associated with tarsal tunnel syndrome so it is strongly suggested that you consult with a podiatrist when they first develop. This type of doctor can properly diagnose and effectively treat this condition.
Tarsal tunnel syndrome may not be a commonly known ailment, but have you heard of carpal tunnel syndrome? Carpal tunnel affects the hands while tarsal tunnel syndrome occurs in the feet and can cause pain and discomfort. Research has indicated that people who have arthritis may be prone to developing this condition, in addition to frequently enduring high-stress activities. Some of the symptoms that are associated with this ailment often include tired feet and ankles, and the overall foot may be numb or have tingling sensations. Some patients have pain in the Achilles tendon area, and the ankles may appear swollen. There are several symptoms that can be associated with tarsal tunnel syndrome so it is strongly suggested that you consult with a podiatrist when they first develop. This type of doctor can properly diagnose and effectively treat this condition.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Why Does My Child Walk on Their Toes?
By monitoring a child’s foot development in the early years—and intervening if any structural abnormalities or dysfunction is present—the child’s quality of life can be vastly improved, and serious foot complications later in life may be avoided. Some milestones in a child’s early development are: sitting up by themselves at approximately 6-7 months, beginning to walk at roughly 12 months, and walking heel-to-toe by age 3 instead of on their toes as some toddlers do while learning to walk. Toe walking after age 3 may just be a habit, or due to a tight Achilles tendon, or it could possibly be an indicator of a muscular, neurological, or developmental issue the child may have. If you are concerned about your child’s foot development, schedule an appointment with a podiatrist for a full examination and consultation.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019