Connect With Us
Blog
Items filtered by date: March 2022
What Is the Purpose of Foot Arches?
The arch is the curved area in the center sole of the foot. At birth, babies do not have arches in their feet, but most will develop arches over time. Those who don’t develop arches have congenital flat feet, which are usually asymptomatic. It is also possible to develop arches normally and then lose them over time for a variety of reasons. This is known as acquired flat feet, and is often accompanied by foot pain or discomfort. But why do we have arches in the first place? The arch of the foot is a very useful structure. It helps the feet stand, stay balanced, run, walk, and jump by adding flexibility and springiness to the foot. With an arch, the foot is better able to absorb shock from physical activities, and the body’s weight is more evenly distributed around the surface of the foot. If you have flat feet and are experiencing any foot pain, please seek the care of a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
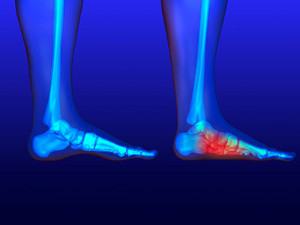
Why Pain From Plantar Fasciitis Is Worse in the Morning
Plantar fasciitis will affect 1 in 10 people, mostly between the ages of 40-60, or younger if they are runners, athletes or dancers. The plantar fascia is the web-like fibrous tissue connecting the heel bone with the toes on the sole of the feet. Stress, micro-tears or other damage to the plantar fascia can cause it to become inflamed, which results in plantar fasciitis. This inflammation, in turn, causes the plantar fascia to tighten during periods of rest or inactivity and typically produces a sharp, stabbing pain towards the middle of heel, where the plantar fascia attaches to it. Initially, once activity is resumed (after waking in the morning, for example), and the plantar fascia begins to stretch, the pain may subside, but will reoccur later in the day. Contributing factors to plantar fasciitis include obesity, foot structure disorders such as flat feet or high arches, having to stand for prolonged periods, and participating in sporting activities with repetitive stress on the plantar fascia (i.e., running and jogging). If you have heel pain, it is a good idea to make an appointment with a podiatrist who can determine if plantar fasciitis is the cause and create a treatment plan to reduce your pain and help repair the plantar fascia.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What Is Wound Debridement?
 A diabetic foot ulcer (DFU) is a type of wound that can develop on the lower limbs of people with diabetes. These wounds typically heal slowly and poorly and are at an increased risk of becoming infected. Sometimes debridement is necessary to treat a DFU. Debridement is the process of removing dead or damaged skin, tissue, and debris from a wound to help it heal. During debridement, the podiatrist will clean and disinfect the wound, then probe it with a metal instrument to check how deep the wound is and if there are any foreign objects in it. The podiatrist will then cut away dead tissues and wash out the DFU. This is generally done under local or general anesthesia. Not all debridement involves cutting away dead tissues. Depending on the needs of the patient, it may also be possible to debride the wound with special enzymes, dressings, and more. If you have DFUs, it is suggested that you are under the care of a podiatrist.
A diabetic foot ulcer (DFU) is a type of wound that can develop on the lower limbs of people with diabetes. These wounds typically heal slowly and poorly and are at an increased risk of becoming infected. Sometimes debridement is necessary to treat a DFU. Debridement is the process of removing dead or damaged skin, tissue, and debris from a wound to help it heal. During debridement, the podiatrist will clean and disinfect the wound, then probe it with a metal instrument to check how deep the wound is and if there are any foreign objects in it. The podiatrist will then cut away dead tissues and wash out the DFU. This is generally done under local or general anesthesia. Not all debridement involves cutting away dead tissues. Depending on the needs of the patient, it may also be possible to debride the wound with special enzymes, dressings, and more. If you have DFUs, it is suggested that you are under the care of a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Julie Jurd-Sadler, DPM from Progressive Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Achilles Tendon Disorders
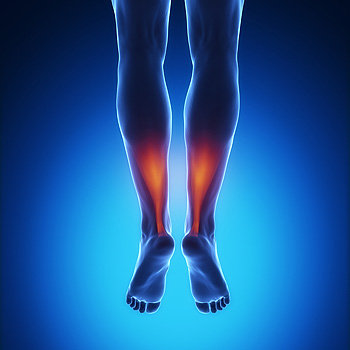 The Achilles tendon is a thick band of fibrous tissue that runs along the back of the lower leg, connecting the heel bone to the calf muscles. When the Achilles tendon is injured, resulting symptoms may include pain, aching, stiffness, soreness or tenderness in the heel or back of the leg, enlargement of the tendon, and damage to the surrounding tissues. There are two main types of Achilles tendon disorders – Achilles tendonitis and Achilles tendonosis. Tendonitis is a typically short-lived inflammation of the tendon. Tendonosis, which can evolve from tendonitis if the former is not treated promptly, can lead to tears in the tendon and degeneration over time. If you have symptoms of an Achilles tendon injury, it is suggested that you consult with a podiatrist.
The Achilles tendon is a thick band of fibrous tissue that runs along the back of the lower leg, connecting the heel bone to the calf muscles. When the Achilles tendon is injured, resulting symptoms may include pain, aching, stiffness, soreness or tenderness in the heel or back of the leg, enlargement of the tendon, and damage to the surrounding tissues. There are two main types of Achilles tendon disorders – Achilles tendonitis and Achilles tendonosis. Tendonitis is a typically short-lived inflammation of the tendon. Tendonosis, which can evolve from tendonitis if the former is not treated promptly, can lead to tears in the tendon and degeneration over time. If you have symptoms of an Achilles tendon injury, it is suggested that you consult with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
What Causes Bunions?
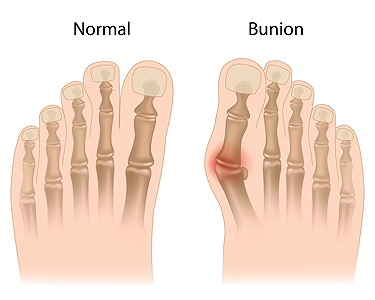 A bunion is a bumpy outgrowth that develops at the joint of the big toe as a result of a deformity known as hallux valgus. The most common symptom is the big toe pushing inward toward the second toe, thereby pushing the joint out of alignment and causing the bump. The main cause is wearing shoes that are pointy or too tight in the toe box. Tight shoes strain the MTP (metatarsophalangeal) joint where the big toe meets the foot. Women are more likely to develop bunions because they often wear high heels. A bunion can also be the result of heredity or arthritis. If you have developed a bunion, it is wise to consult with a podiatrist earlier rather than later. The podiatrist can examine the area and help you decide the correct measures to take. Treatment ranges from elastic bunion pads or shoe inserts in minor cases to surgery in the most severe.
A bunion is a bumpy outgrowth that develops at the joint of the big toe as a result of a deformity known as hallux valgus. The most common symptom is the big toe pushing inward toward the second toe, thereby pushing the joint out of alignment and causing the bump. The main cause is wearing shoes that are pointy or too tight in the toe box. Tight shoes strain the MTP (metatarsophalangeal) joint where the big toe meets the foot. Women are more likely to develop bunions because they often wear high heels. A bunion can also be the result of heredity or arthritis. If you have developed a bunion, it is wise to consult with a podiatrist earlier rather than later. The podiatrist can examine the area and help you decide the correct measures to take. Treatment ranges from elastic bunion pads or shoe inserts in minor cases to surgery in the most severe.
If you are suffering from bunions, contact Julie Jurd-Sadler, DPM of Progressive Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Ijamsville and Mouth Airy, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019